Gail and Joseph Berardino
Gail and Joseph Berardino have each built illustrious careers in textiles and the financial world matched only by their prolific commitments to service and philanthropy. Gail Berardino retired from McCall Pattern as Vice President of Advertising and Promotion and Publisher of Vogue Patterns Magazine after a twenty-five-year career. Joe Berardino, a graduate of Fairfield University, has been a Managing Director of Alvarez & Marsal in New York City since 2008. Previously, he served as Chief Executive Officer of Andersen Worldwide and he has served on several private and public company boards.
The couple each joined the Order of Malta, American Association in 2004. Together, they co-chaired the Order’s 25th Annual Pilgrimage to Lourdes in 2010 and currently co-chair the Order’s “Called to Serve” capital campaign. Gail Berardino has served as Hospitaller and a member of the Order’s board of councilors. Presently, she serves on the Malta Human Services foundation board and the Holy Family Hospital of Bethlehem foundation board. Located in the West Bank, Holy Family Hospital facilitates Israeli – Palestinian cooperation in the medical field. The hospital delivers 4,800 babies annually. Since 1990, 90,000 infants have been born. No one is ever turned away.
Gail Berardino presently serves on the advisory board of the Fairfield University School of Nursing. Joe Berardino has served a total of eighteen years on the Fairfield University board of trustees, chairing the advancement and finance committees. Together, the couple has served as mentors for the University’s Ignatian Residential College for sophomores. Each year, the Berardino’s sponsor nursing students to join the Order of Malta Lourdes Pilgrimage as a capstone internship experience to complement their nursing studies. The Berardino’s also support Jesuit higher education through endowed scholarships. Joe Berardino presently serves on the University of Maryland School of Medicine’s Institute of Human Virology. They are active in their home parish of Saint Michael the Archangel in Connecticut, and they volunteer at Parsonage Cottage, an assisted living community for the elderly.
It is Catholic Guardian Services’ great privilege to honor Gail and Joseph Berardino with the Child of Peace Award at the 36th Annual Child of Peace Awards Celebration.
John W. Tietjen
A native New Yorker, John W. Tietjen retired after a distinguished career in the banking industry, most recently serving as the Chief Financial Officer of the New York Stock Exchange listed Sterling Bancorp. His expertise in banking, accounting, and finance contributed to the successful merger of Sterling National Bank and Provident Bank in 2013.
A graduate of Archbishop Molloy High School and Iona College, John is steeped in Catholic education and the importance of service to the community. His belief in the Catholic value of supporting those who are underserved and under-resourced led him to join the board of Catholic Guardian Services in 2014. He has applied his extensive business experience as a member and, subsequently, as co-chair of Catholic Guardian’s audit committee. Additionally, he serves on the finance committee, charged with ensuring the agency’s ability to support its mission despite shifts in governmental support and slow economic growth.
Throughout 2020, John served on special board committees, working with the agency’s management team to provide an effective and swift response to the evolving threat of the COVID-19 pandemic. His careful guidance assisted the agency in carrying out its critical responsibilities of ensuring the health of the children and families served by Catholic Guardian and the health of the staff—while maintaining a robust suite of frontline safety net programs and services and developing new services as warranted by the crisis.
John is a longtime financial supporter of Archbishop Molloy High School, Iona College and the Children’s Aid Society of New York, an organization that shares a similar mission to Catholic Guardian Services. He is a benefactor of a non-profit literacy program, Libros para Pueblos, based in Oaxaca, Mexico. He served on the board of the Cancer Support Team in Westchester County, was a member of the finance committee and chaired the governance and nominating committee, and volunteers at New York-Presbyterian Lawrence Hospital in Bronxville, N.Y.
It is Catholic Guardian Services’ great privilege to honor John W. Tietjen with the Humanitarian Award at the 36th Annual Child of Peace Awards Celebration.
Frontline Heroes




Catholic Guardian Services’ teams of case planners, social workers, clinicians, nurses, therapists, direct care professionals, and administrators who served on the frontlines of the COVID-19 crisis.
Since 1887, Catholic Guardian Services has been helping build stronger families and healthier communities by providing holistic human services for children and families, regardless of race, religion, creed, or life circumstances. The populations we serve include families in crisis, expectant mothers and new parents, children in the child welfare system, families in need of mental health care, youth within or soon-to-be-leaving foster care, individuals with intellectual or developmental disabilities, unaccompanied minor children immigrating to the U.S. and seeking asylum, and families at risk of being overwhelmed by the toxic stress of poverty.
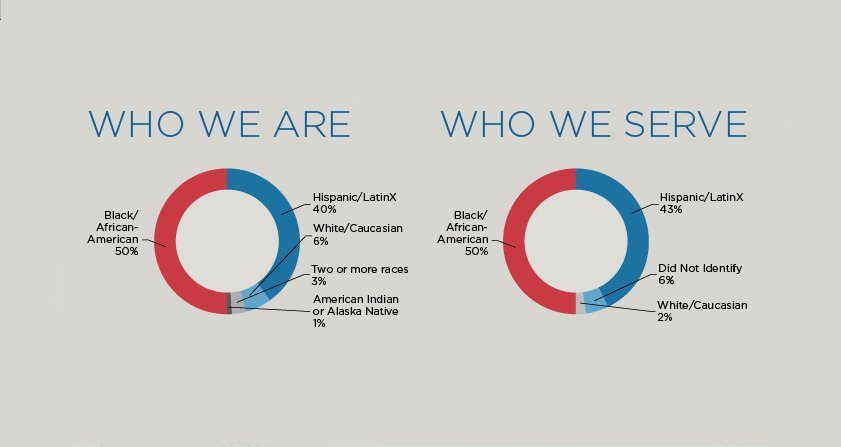
Our workforce is comprised of just under 700 full-time employees each of whom is an essential worker and contributed on the frontlines of the COVID-19 crisis. 50% of our workforce self-identify as Black or African American, 40% as Hispanic, 6% as white, 3% as mixed-race, and 1% as indigenous American. Many of our frontline heroes live in the communities where they work and are neighbors with the families receiving support within our community of care.
When New York State was on PAUSE in 2020, Catholic Guardian’s teams did not miss a single moment of providing essential services to children and families throughout New York City. Without hesitation, our staff prioritized the health and safety of the families within our community of care and developed systems and protocols to keep everyone safe while, at the same time, being the human safety net for children and families in need.
It is Catholic Guardian Services’ great privilege to honor our teams of case planners, social workers, clinicians, nurses, therapists, direct care professionals, and administrators who served on the frontlines of the COVID-19 crisis with the Rosalie Cadron-Jetté Award for Courage and Compassion at the 36th Annual Child of Peace Awards Celebration.
Twilight Sleep, Barbarism and, Dr. Joseph DeLee:
Midwifery and Obstetrics in U.S.
Midwifery has been the dominant form of maternal health and birth practice throughout most of human history. Biological Anthropologists estimate that midwives have been active for more than one million years. By the mid-twentieth century, however, this practice changed dramatically in the United States. During and after World War I, immigration limits reduced the supply of both foreign-trained midwives and foreign-born women, their most loyal clientele. At the same time, physicians were becoming better educated and increasingly esteemed and preferred among the middle and upper classes with the rise of modern medicine. Obstetric anesthesia and “Twilight Sleep”—a popular twentieth-century procedure in which women entered a state of drug-induced sleep during labor and awoke after birth with no recollection of the procedure—symbolized medical progress. This led to collective defamation of midwifery as an antiquated relic of the poor and uneducated classes. Thus, despite facilitating approximately half of all births in 1900, midwives attended less than 15% by 1935.
Furthermore, in 1915, The Association for the Study and Prevention of Infant Mortality published a paper in which Dr. Joseph DeLee declared midwifery a “a relic of barbarism” and described childbirth as a pathological process from which few women escape “damage,” leading to a growing perception among his contemporaries that nearly all births required intense medical intervention by default. As a result, preemptive sedation, episiotomies, and prophylactic birthing forceps all quickly became routine practice in obstetrics, but safety was not improved. Maternal mortality remained flat in the following decades despite decreases in tuberculosis death rates, and infant mortality due to birth injuries increased 41% between 1915 and 1929 because of excessive obstetric intervention.
In the early 1970s, however, women’s groups began advocating for autonomous, gynecological self-care and encouraged a revival of lay midwifery, arguing that obstetrics and women’s health needed to be demystified and de-medicalized. This led to the founding of The Midwives Alliance of North America (MANA) in 1982, and in 1992, the governor of New York signed a new Professional Midwifery Practice Act into law which defined and legitimized midwifery as a profession. Midwifery has been steadily increasing in popularity as a primary birth method since then, from 3.2% of all U.S. deliveries in 1989 to 9.4% in 2018.
Today, most midwives in the U.S. are certified nurse-midwives: registered nurses with advanced gynecological and obstetrics training as well as a master’s degree in nurse-midwifery who function much like nurse practitioners and refer patients to physicians whenever necessary. 97% of midwives practice in hospitals, and thirty-three states, including New York, mandate that insurance companies reimburse the cost of hiring a nurse-midwife. Clinical research suggests that midwives are a compelling option for mothers with low-risk pregnancies—which account for 85% of all U.S. pregnancies—to consider. Studies have shown that using a midwife can lead to less time spent in labor, lower infant mortality, greater maternal satisfaction, higher time- and cost-efficiency, fewer unplanned cesarean sections, and fewer preterm deliveries, episiotomies, and instrumental births. In addition, in Denmark, Sweden, and The Netherlands, where midwives deliver almost all babies, infant mortality rates remain much lower than in the U.S.
Doulas, trained birthing assistants who are neither part of the hospital staff nor the mother’s social network, can further improve these outcomes. A major meta-analysis found that women who receive continuous support during childbirth from doulas are 15% more likely to have a spontaneous vaginal birth, 39% less likely to receive an unplanned cesarean section, and 31% less likely to report negative feedback about their experience. They also spend 41 fewer minutes in labor on average, and their babies were 38% less likely to receive a low five-minute Apgar score, a neonatal health assessment performed 1 and 5 minutes after birth. In addition, Swedish oxytocin researcher Dr. Kristin Uvnas Moberg writes that the presence of a doula increases the production of natural pain-coping hormones (beta-endorphins) and enhances oxytocin release, which decreases the mother’s stress reactions, fear, and anxiety, and increases contraction strength and effectiveness.
Given that the U.S. is one of just eight countries globally that exhibited increases in maternal mortality between 2003 and 2013, improving maternal health remains particularly urgent. Increasing collective acceptance and prioritization of midwifery may be a strong first step: for instance, the U.S. has 84% fewer midwives per 1,000 live births compared to the Netherlands, and our maternal mortality rate is nearly five times higher. Further, the “Listening to Mothers” survey found that while most mothers used an obstetrician for their prenatal care and delivery, more than half said they would definitely want (17%) or would consider (37%) a midwife for a future pregnancy.
The primary determinant in any birth plan should always be the expectant mother’s specific needs, circumstances, and preferences, especially considering that heightened maternal stress can itself increase the risk of low birth weight. A midwife can be an excellent option for low-risk pregnancies, but a trusted OB-GYN can be just as strong a choice, and a doula can prove a tremendous help in either case.
Early Prevention and the U.S. Mental Health Crisis
Mental health disorders are the most common diseases of childhood. Of the 74.5 million children in the United States, an estimated 17.1 million have or have had a psychiatric disorder — more than the number of children with cancer, diabetes, and AIDS combined. While public perceptions and common knowledge about mental illness have improved drastically in recent decades, gains have proven to be far fewer and further between in outcomes and care delivery, especially for U.S. children and adolescents. In the United States, 17% of children ages 2-8 years old, 20% of adolescents 13-18, and 29% of young adults 18-25 live with a mental health disorder. By age 17, 36% of girls have experienced depression, and suicide rates for every male age group under 75 years old have increased since 1999. Between 2007 and 2016, emergency room visits among children who committed deliberate self-harm rose 329%. Suicide remains the second leading cause of death for all age groups under 35 in the U.S. Mental and behavioral health problems are responsible for more than 40 million years lived with a disability among 20 to 29-year-olds worldwide, and, coupled with substance abuse disorders, claim 184 million DALYs (disability-adjusted life years, an aggregate measure of mortality and burden of disease) annually.
Tragically, the U.S. mental healthcare system has not kept up with this acceleration. 50% of Americans will meet the criteria for a diagnosable mental health condition at some point in their life, and half will do so before age 14, but 70% of children and adolescents who experience mental health problems do not receive appropriate interventions at a sufficiently early age, and 49% receive no treatment whatsoever. Roughly 50% of Americans with severe psychiatric disorders, some 3.5 million people, are receiving no treatment for their conditions, and even if they were to seek help of their own volition, it takes nearly four weeks of active pursuit on average to meet with a qualified psychiatrist. As a result, the average delay between the initial onset of symptoms and professional intervention for an individual in need is ten years.
Costs, too, have skyrocketed in recent decades. The U.S. spends $201 billion on mental healthcare every year, more than any other medical condition, including diabetes, kidney disease, and hypertension combined. Untreated mental illness costs the U.S. up to $300 billion more in lost productivity. The total economic burden of depression alone tops $210 billion, and, like other mental illnesses but unlike most diseases, most of this is comprised of indirect rather than direct costs. Globally, mental disorders are on the rise in every country, accounting for an estimated 12 billion lost workdays each year and a projected global economic cost of $16 trillion between 2011 and 2030, a figure equivalent to 77% of U.S. GDP in 2020.
Fortunately, early prevention programs have the potential to greatly improve psychological, medical, and socioeconomic outcomes for children and adolescents facing mental health challenges, produce substantial long-term economic benefits, and provide vital quality of life improvements for affected individuals and their families. Improving the mental health of a single child can save the U.S. $140,000 over his or her lifetime, and evidence-based psychotherapy modalities such as Cognitive Behavioral Therapy for children and adolescents with anxiety can offer long-term returns of up to $23.57 per dollar invested and boast a 95% chance of total benefits exceeding total program costs. For figures as low as $81 per child per year, early childhood prevention programs can offer superior recovery and empowerment opportunities for children in need of intervention, empowering them for future health, independence, and success. These modalities are also effective at preventing future mental health-related hospitalizations, which cost $15,318 per average stay of 7.2 days, and incarceration, which costs New York taxpayers $167,731 per inmate per year and leads to a 54% recidivism rate among those with severe mental illnesses. These outcomes are no rarities, either: 70% of youth in state and local juvenile justice systems have a mental illness, and suicide rates among youth in juvenile justice facilities are over three times that of their peers in the general population despite constant supervision, minimal access to deadly weapons, and growing awareness of inmates’ elevated risk levels.
Early prevention programs such as those administered by Catholic Guardian Services drastically improve children and families’ quality of life, prevent tragic and costly outcomes throughout adolescence and early adulthood, and foster healthy, informed, and consistent dialogue about mental health.